Authors: Ranjeet Dhonkal (contact: Ranjeet.Dhonkal@haw-hamburg.de), John Middleton (United Kingdom), Ralf Reintjes (Germany), Laurent Chambaud (France), Alberto Fernandez (Spain), Jose M Martin-Moreno (Spain), Natia Skhvitaridze (Georgia)
![]()
This page of the ASPHER website is dedicated to policies and descriptions of the state of the emergence from lockdown and recovery from the pandemic in different countries. It is a dynamic page - material will be published here as it becomes available. If you would like to contribute, please contact the ASPHER secretriat or Ranjeet.Dhonkal@haw-hamburg.de directly.
![]()
Relaxation from lockdown
The coronavirus disease (COVID-19) pandemic has impacted massively on all aspects of economic, social and educational life. It has affected children and families and adversely impacted on older people, people with disability and vulnerability to infection. Health systems have been stretched to their limits and the personal safety of health and care workers and other key workers is being threatened. Businesses and borders have been closed down.
The immediate priority of the countries is to fight and prevent the spread of COVID-19 pandemic and limit the weakening of socio-economic consequences at most. Many countries are now tentatively addressing the first steps to lighten the effect of country-wide lockdown, to seek to recover, resetting their economies, safely, without awakening a second wave of the pandemic.
There are a number of key documents relating to the path from lockdown. The most significant from the European viewpoint are the WHO Europe key considerations and the EU roadmap.
ASPHER supports the WHO Europe key considerations for the gradual easing of the lockdown restrictions in response to the spread of COVID-19 across the European Region.
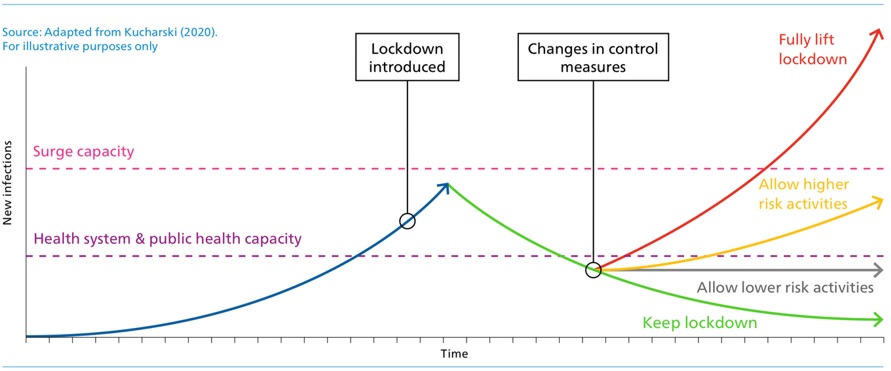
The transition out of lockdown is complex and involves judgements which must balance the potential for a second catastrophic wave of infection, versus continued damage to health through lockdown measures, and through damage to the economic and social fabric of societies.
WHO Europe describes 4 key components for the consideration of easing large-scale restrictive public health measures:
- public health and epidemiological measures;
- capacity for dual-track health system management;
- population and behavioural insights; and
- social and economic implications.
WHO Europe guidance includes 6 criteria for moving to ease lockdown restrictions. Countries must ensure:
- Evidence shows that COVID-19 transmission is controlled.
- Sufficient public health and health system capacities are in place to identify, isolate, test and treat all cases, and to trace and quarantine contacts.
- Outbreak risks are minimized in high-vulnerability settings, such as long-term care facilities (i.e. nursing homes, rehabilitative and mental health centres) and congregate settings.
- Preventive measures are established in workplaces, with physical distancing, handwashing facilities and respiratory etiquette in place, and potentially thermal monitoring.
- Manage the risk of exporting and importing cases from communities with high-risks of transmission.
- Communities have a voice, are informed, engaged and participatory in the transition.
The Joint European Union Road Map towards lifting COVID-19 containment measures sets out three sets of criteria relevant to assess whether the time has come to begin to relax the confinement.
Epidemiological criteria showing that the spread of the disease has significantly decreased and stabilised for a sustained period of time. This can, for example, be indicated by a sustained reduction in the number of new infections, hospitalisations and patients in intensive care.
Sufficient health system capacity, in terms of, for instance, occupancy rate for Intensive Care Units, adequate number of hospital beds, access to pharmaceutical products required in intensive care units, the reconstitution of stocks of equipment, access to care in particular for vulnerable groups, the availability of primary care structures as well as sufficient staff with appropriate skills to care for patients discharged from hospitals or maintained at home and to engage in measures to lift confinement (testing for example).
Appropriate monitoring capacity, including large-scale testing capacity to detect and monitor the spread of the virus combined with contact tracing and possibilities to isolate people in case of reappearance and further spread of infections. Antibody detection capacities, when confirmed specifically for COVID-19, will provide complementary data on the share of the population that has successfully overcome the disease and eventually measure the acquired immunity.
The EU believes three basic principles should guide the EU and its Member States: (1) Action based on science, with public health at its centre; (2) Action coordinated between the Member States: and (3) respect and solidarity between Member States.
For the USA, American Enterprise Institute has set four similar criteria for coming out of lockdown:
- The number of new cases has declined for at least 14 days.
- Rapid diagnostic testing capacity is sufficient to test, at minimum, all people with COVID-19 symptoms, as well as close contacts and those in essential roles.
- The healthcare system is able to safely care for all patients, including having appropriate personal protective equipment for healthcare workers.
- There is sufficient public health capacity to conduct contact tracing for all new cases and their close contacts, as described in the National Plan to Enable Comprehensive COVID-19 Case Finding and Contact Tracing in the US.
The public should be encouraged to maintain the new normal of hand hygiene, coughing etiquette and distancing routines. In addition, the health workforce needs to be offered the opportunity to rest and recuperate. Understandably, COVID-19 has had an effect on routine service delivery by crowding out other health issues that health systems will need to quickly address. For example, children may have missed routine vaccinations, which will need to be quickly rectified to avoid any outbreaks of vaccine-preventable diseases.
The public health community and the people we serve, must all be able to respond to any new outbreaks of COVID-19.
Further, for the State of New York, Governor Andrew Cuomo has introduced seven criteria for easing lockdown in different regions of the State.
An example of the dashboard for achieving these measures is shown here.
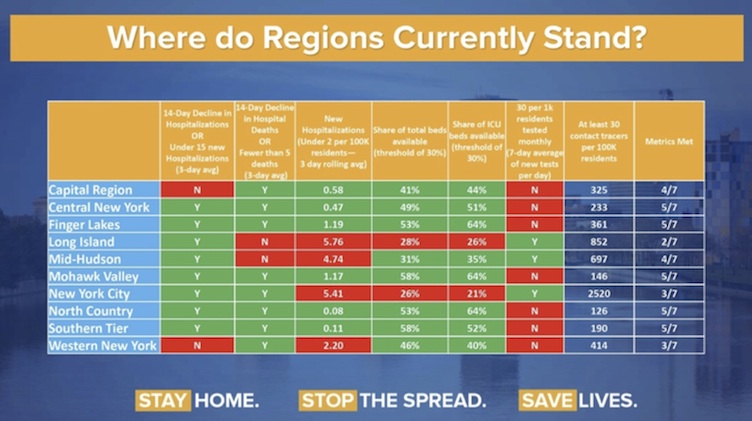
Cuomo A. May 4th 2020. Where do Regions currently stand? https://twitter.com/NYGovCuomo/status/1257342748891459584/photo/1
Key references:
![]()
Cross-country analysis
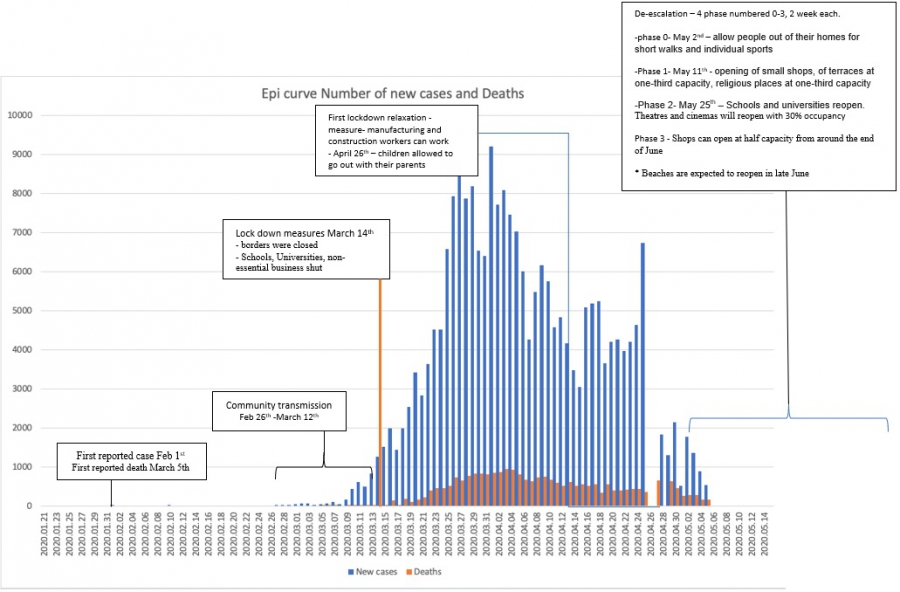
Spain
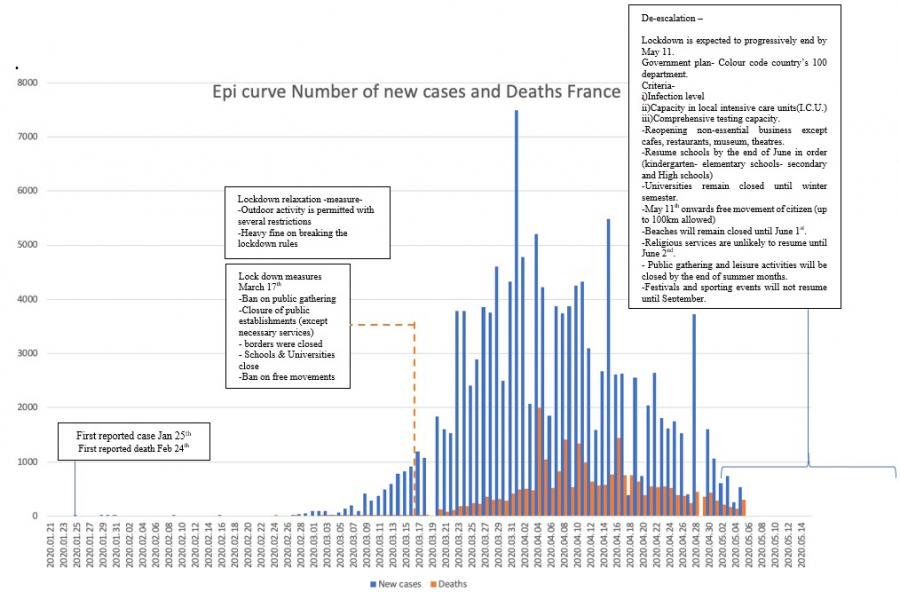
France
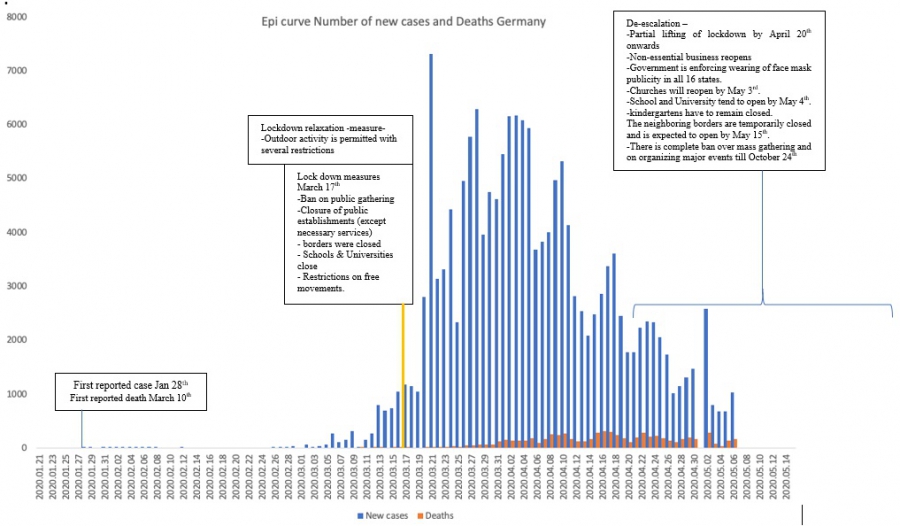
Germany
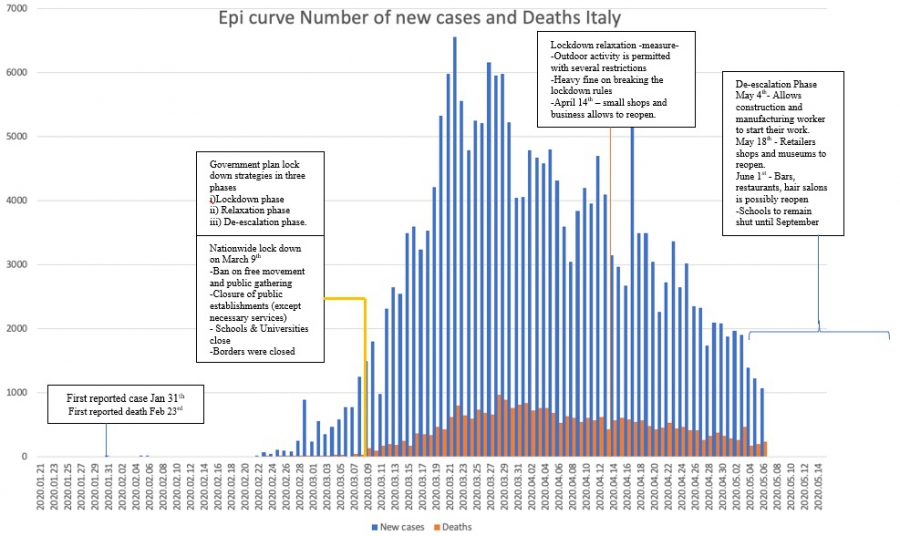
Italy
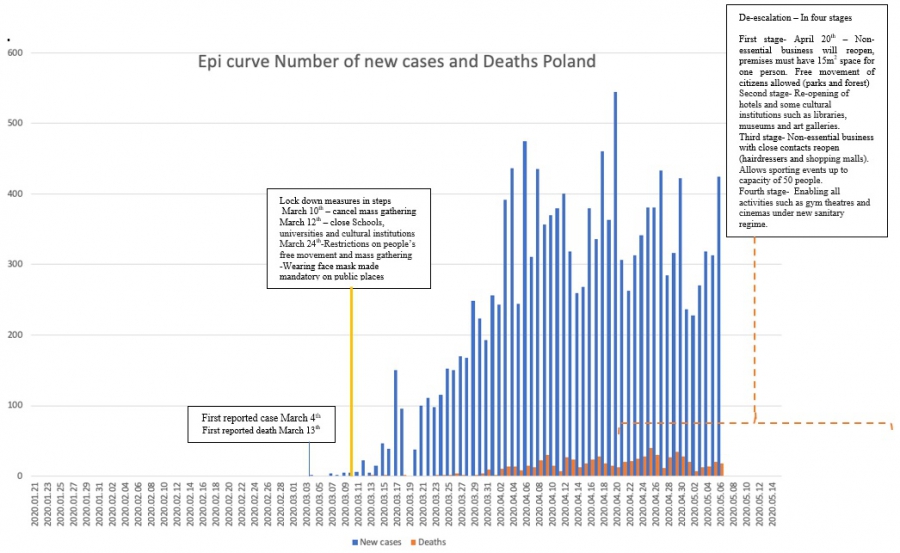
Poland
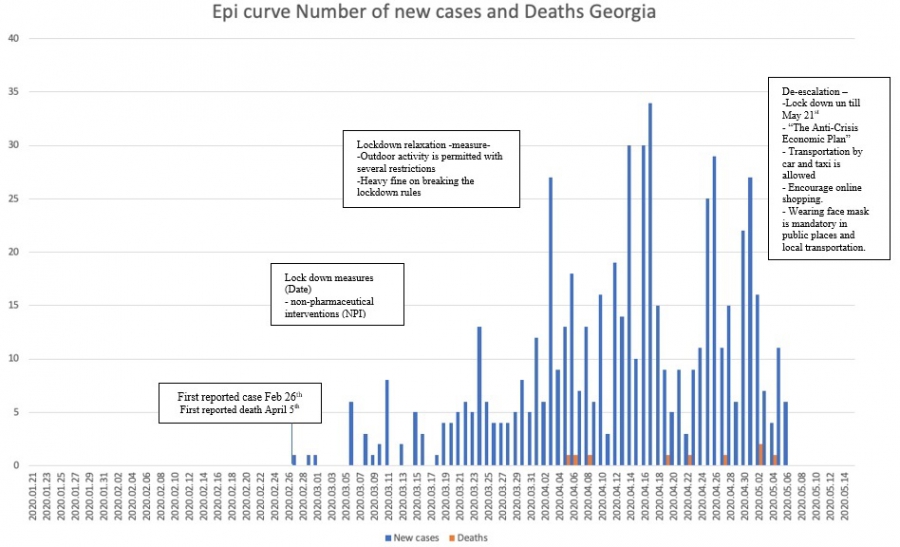
Georgia
United Kingdom

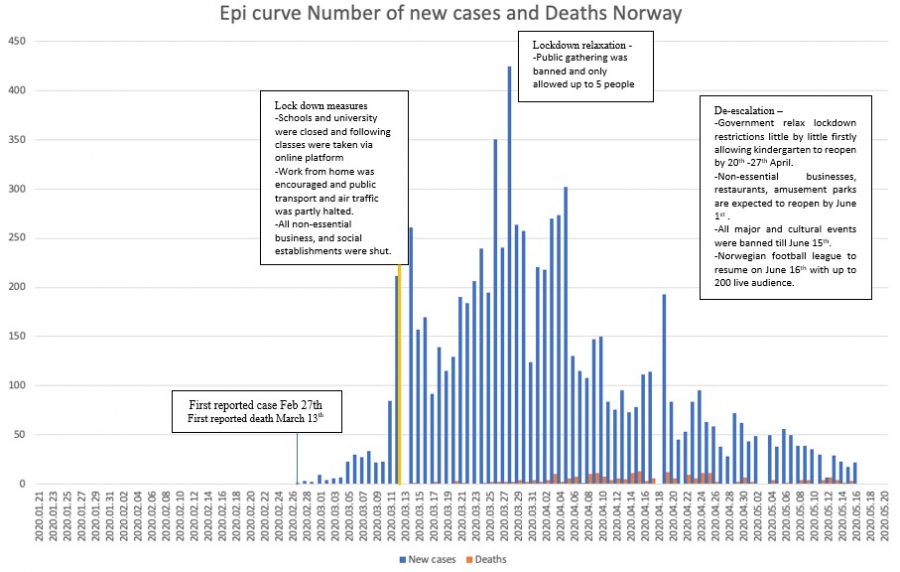
Norway
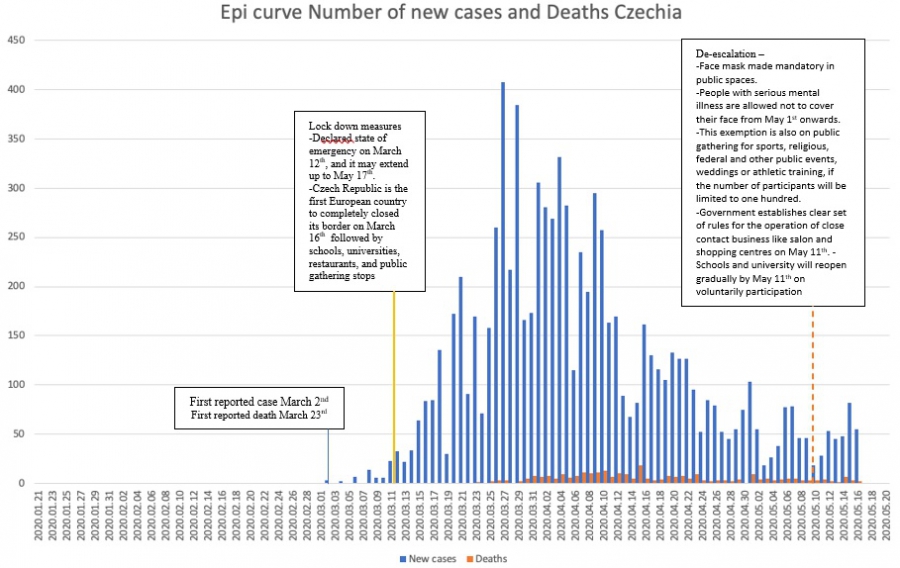
Czech Republic
![]()
ASPHER conclusions so far
In accordance with the WHO EURO and EU recommendations we believe there should be:
- Planned and gradual lifting
- Protection of groups of people needing special care
- Lifting measures should be divergent in approach
- Public gathering should be permitted
- Preventive measure should be sustained
- Proper monitoring of measures
- In addition, recovery of health and care services
Planned and gradual lifting
Essential and reasonable approach for planned and gradual lifting of coronavirus containment measures should be controlled, slow and in step wise manner. Sufficient time should be left between the steps considering one incubation period to identify and adverse effects. Time interval between relaxation may varies and can be more than one incubation period cycle as it strongly depends on the quality of surveillance system and countries capacity to measure the effects.
WHO and the EU also suggest the easing of restrictions in certain countries will have to be staggered over a period of time. Due to the nature of COVID-19, it is difficult to understand any adverse impact of easing of restrictions until 10–14 days have passed.
As restrictions are eased, it is important for countries to recognize that it may be necessary to reintroduce physical distancing measures to manage outbreaks at short notice. John Hopkins policy advisers recommend 'a state should revert to lockdown and continue “slow the spread” if a substantial number of cases cannot be traced back to known cases, if there is a sustained rise in new cases for five days, or if hospitals are no longer able to safely treat all patients requiring hospitalization’. WHO Europe calls this ‘bidirectional working’. Countries will need to be adaptable, and secure a high level of public understanding and support for further control measures if needed.
Target group needs special care
Protection of most vulnerable populations should be central in the decision to maintain or lift measures. People aged ≥70 and people of any age who have serious underlying medical conditions (for example - heart disease, hypertension, diabetes, chronic respiratory disease, cancer), at risk due to compromised immune system from medical condition or treatment (for example - chemotherapy) might be at higher risk for severe illness from COVID-19. People with mental illness are another possible risk group. People with either mild symptoms or severe should be advise to stay quarantine as will help the break the chain of transmission.
Lifting measures should be divergent in approach
Lifting measures should start with an approach targeting the local area first by allowing the functioning of the internal market and on free movement of the people. After careful observation and monitoring the measures gradual lifting should extend to broader geographical coverage. The travel restrictions should be lifted once physical distancing rules are widely and responsibly applied. External border reopening and access of non-EU residents to the EU should happen in later stages. The widely used 14 day quarantining of airline travellers on arrival into another country is a sensible precautionary measure.
Public gathering should be permitted on a staged basis
Public gathering should be progressively permitted. It is important to determine the appropriate sequence for reintroduction of gatherings. The EU road map describes such gatherings in terms of: (i) Schools and universities; (ii) Nonessential business; (iii) Social activities; (iv) Mass gathering.
The EU is silent on religious gatherings. For some this is the most heart-breaking problem of the pandemic- not being able to properly mourn the loss of their loved ones. For the present, assessment of conduct of ceremonies, births, marriages and funerals will need to be determined in the context of risk assessments. These are the same principles which apply to all public gatherings. It is important to recognise the impacts of public gathering beyond the confines of the facility in which the gathering is taking place - impacts for public transport, for car parking, for gatherings outside the facility, for hospitality facilities, for the length of time of the event and for the ease of access and egress. The potential for ticketing and reservations as a means to control numbers is another consideration. Potential use of remote technologies should also be considered. Another consideration is the capacity of the event organisation to provide, or police personal hygiene measures Detailed risk assessment is required in each case.
Preventive measures must be sustained
Health promotion and health awareness campaign should encourage people to maintain good hygiene practice ‘the new normal’ (use of sanitizers, washing of hands, coughing/sneezing etiquette, cleaning high-contact surfaces, etc.). In addition, employers should discourage the previous culture of ‘presenteeism’ in which employees were obliged to work, or colluded inworking, even if ill and especially when infectious to others. Through these awareness campaigns people should be provided with brief information regarding risk assessment. ASPHER recommends the use of non-surgical facemasks or face coverings in the community. This is especially the case when visiting busy, confined spaces, such as grocery stores, shopping centres, or when using public transport. The European Union has also adopted the recommendation as made by the European Centre for Disease Surveillance and Control.
Proper monitoring of measures.
WHO recommends a rigorous surveillance programme to identify, test and isolate all cases and to trace and quarantine their contacts is vital to ensure that localized outbreaks do not get out of control. ASPHER agrees and has set out its view on testing; nevertheless, there are concerns about the real world effectiveness of the tests in picking up true infections, and in over-estimating population exposure in mass serology.
In addition to testing regimes, novel and lateral sources of surveillance data should be used. These may be different from country to country. Under-reporting of COVID deaths may be off-set by use of the excess mortality indicators available for some countries. Other primary care data, COVID and respiratory data may be available and add to a picture of the state of the outbreak for particular countries.
When measures are eased, cases should not exceed a sustained reproductive factor of 1, and should ideally remain below 1. This means that a person with confirmed COVID-19 does not pass the disease on to more than 1 other person to keep the number of cases flat. For example, Germany used an R factor of 0.7 before reducing its restrictions.
Recovery of health and care services
We must recognise and celebrate health and care services workers; and we must mourn and honour the colleagues we have lost. We must also recognise and make provision for a level of mental distress, post traumatic stress disorder amongst health and care workers and recongise that restarting health and care services to full capacity will not be possible. We must also plan for a recovery of non urgent health care and some urgent and routine care which has been put on hold during the pandemic. We will also have built up waiting lists and demand for health services during the pandemic period and we may not have planned for lockdown induced illness, (e.g., domestic violence), economic inequality induced illness (unemployment related suicide) and vulnerability induced illness (care for homeless and migrant people). We should plan for full reinstatement of life saving preventive care, like the childhood immunisation programmes, maternal and reproductive health care, and long term conditions management in primary care.
![]()
Ongoing & further work
More work is being/will be done by ASPHER members over the coming days on:
Ensuring that personal hygiene habits for public interactions are properly introduced and disseminated
- New norms of frequent hand washing, coughing etiquette, and physical distancing
- Use of appropriate masks in all relevant public spaces – particularly when indoors where the safety distance cannot be maintained
- Glove use is advisable only for certain occasions or jobs where they are recommended according to protocol. In other cases, they cannot substitute for hand washing and the gloves themselves can become a vector of contagion.
Protecting people at standard workplaces
- Workplace risk assessment (teamwork with appropriate worker representation)
- Structural preventive measures
- Non workplace options where possible
- Access to work - public versus private transport
- Presenteeism not tolerated - ‘new norm of not being ill at work’
- Age group selection for workers
Taking care with particular attention to vulnerable groups
- Black and minority ethnic issues
- Mental health needs of people in lockdown
- Domestic violence
- Elderly (particularly at nursing/care homes)
Ensuring the right conditions to reopening activities
- Children’s activities – schools, daycares
- Sport/individual activities
- Cultural activities
Dealing with issues related to education and training in an appropriate and exemplary manner
- Including those of specific relevance to schools of public health
- Also in the area of professional regulation and standards
Rigorously addressing Disease Surveillance
- Contact tracing
- Surveillance apps
- Serological testing
- Immunity certifications “passports” and use of tracking applications
- Regional differences in prevalence
Promoting economic recovery with a vision of equity and public health
- Characterization of inequalities and identification of needs
- ...
Key references
ASPHER Statement on the streategic use of masks:
https://www.aspher.org/aspher-statement-masks.html
ASPHER Statment on the COVID-19 testing:
https://www.aspher.org/aspher-statement-covid-19-testing.html
Other references:
https://analysis.covid19healthsystem.org/
https://www.euromomo.eu/graphs-and-maps/
https://www.bmj.com/content/369/bmj.m1557.full?ijkey=C7XsvkvsFLHZc73&keytype=ref
https://www.ft.com/content/6bd88b7d-3386-4543-b2e9-0d5c6fac846c
![]()
 I am Dr. Ranjeet Dhonkal. I have completed my Bachelor's in Dental surgery and at present I am enrolled in a MPH programme at University of Applied Sciences - Hamburg, Germany. My areas of interest are infectious epidemiology, field epidemiology and health policies. Recently I have completed my research on the COVID-19 world pandemic in which I have explored the strategy and preventive measures followed by different European countries to combat this COVID-19 crisis.
I am Dr. Ranjeet Dhonkal. I have completed my Bachelor's in Dental surgery and at present I am enrolled in a MPH programme at University of Applied Sciences - Hamburg, Germany. My areas of interest are infectious epidemiology, field epidemiology and health policies. Recently I have completed my research on the COVID-19 world pandemic in which I have explored the strategy and preventive measures followed by different European countries to combat this COVID-19 crisis.
Key supervisors: John Middleton (ASPHER) & Ralf Reintjes (HAW Hamburg)
![]()